Rapidly Spreading Fungus Already In 28 States, Including Illinois, Presents ‘Urgent’ Threat, CDC War
Posted by admin on
What is the new fungus disease?
The Centers for Disease Control and Prevention (CDC) has issued a warning about a drug-resistant strain of fungus, Candida auris (C. auris), spreading in health care facilities in the United States.
What we know about the deadly fungus Candida auris
One in three patients with invasive infections dies, but it can be difficult to assess the exact role Candida auris played in vulnerable patients, said CDC epidemiologist Dr Meghan Lyman, the report’s lead author.
The most common symptoms are fever and chills that do not improve after treatment, according to the CDC.
Because most patients are already sick, it is sometimes hard to detect the fungal infection. Only a laboratory test can confirm an infection.
The infection was first reported in the US in 2016. The most rapid rise in cases was from 2020 to 2021, according to CDC data which was published in the Annals of Internal Medicine.
Another reason for concern was the increase of cases that became “resistant to echinocandins” which is the antifungal medicine most recommended for treatment of the infection.
The CDC attributes the rise in the number of cases reported to poor infection prevention at healthcare facilities, as well as enhanced screening efforts which have picked up on the surge in infections.
It also may have worsened due to strain on healthcare and public health .
In Mississippi, the state’s lead epidemiologist has identified a long-term acute-care facility to be at the centre of the outbreak.
“Unfortunately, multi-drug resistant organisms such as C. auris have become more prevalent among our highest risk individuals, such as residents in long-term care facilities,” Dr Paul Byers told NBC.
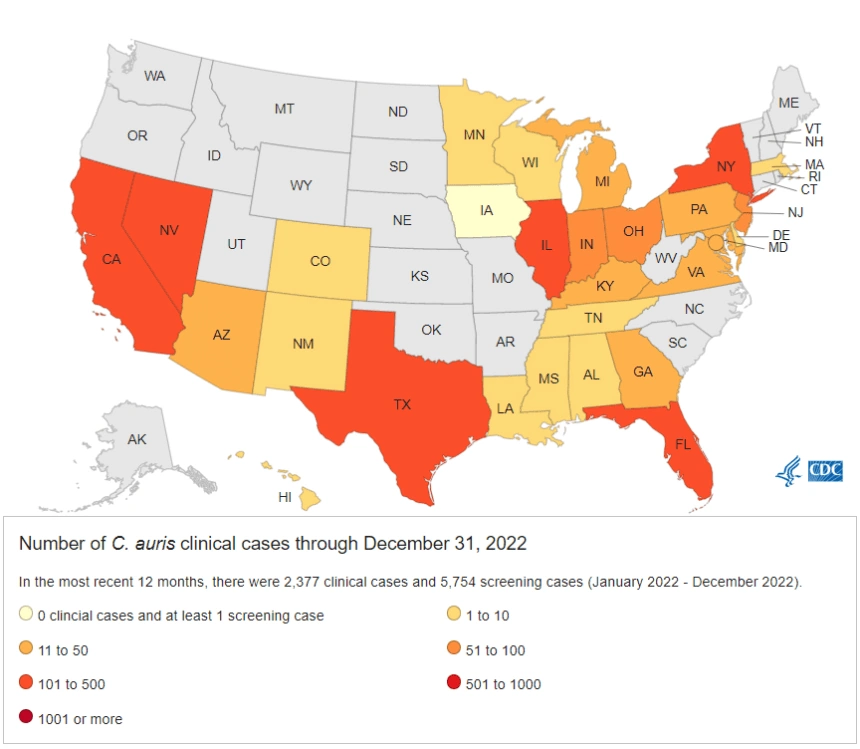
According to preliminary CDC data, there were 5 clinical cases of Candida auris in 2022. In more populous states like California and Texas, there were 359 and 160 cases, respectively.
Nationwide there were 2,377 clinical cases in 2022, which would be a marked rise from the 1,471 cases in 2021.
Dr Lyman, told in 2023 CBS News the rise “emphasises the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control”.
Other countries have also been seeing an increase in Candida auris cases.
Last year, the World Health Organization included it on its list of “fungal priority pathogens”.
Public health experts refer to C. auris as an emerging pathogen, which means an organism that has newly appeared or been discovered but has since rapidly spread — either in terms of cases or countries where it is now reported.
Why is C. auris potentially dangerous?
Dr. Scott Roberts, associate medical director of infection prevention at Yale School of Medicine, told ABC News that C. auris can spread either from person-to-person transmission or by people coming into contact with contaminated surfaces.
“This spreads person to person and we do not think of really any other fungus as spreading person to person in a meaningful way,” he said. “And it’s really hard to kill. Standard Lysol wipes, disinfectant wipes don’t kill it. We need dedicated bleach wipes or additional products geared for Candida auris.”
The other issue is there are strains of C. auris that are drug-resistant, meaning infections caused by the yeast will not respond to multiple antifungal drugs commonly used to treat Candida infections.
How is it diagnosed?
Patients with C. auris infections are typically diagnosed after cultures of blood or other bodily fluids are analyzed.
However, experts said this can be difficult because analyzing these cultures requires updated machines or updated libraries, not all labs of which have the capability.
Additionally, it can be hard to identify C. auris on the culture results and it can be confused with other species of Candida.
“The way cultural results come back, first it’s like, ‘Okay, it looks like yeast,'” said Doron. “Then it’s like, ‘Okay, it looks like Candida’ only it could take days before it’s Candida auris and you may be using the wrong drugs.”
Who is at risk?
Most healthy people do not need to worry about C. auris infections, experts said.
However, those with weakened immune systems or who are immunocompromised are at risk of hard-to-treat infections.
Additionally, nursing home patients or hospital patients who have or have had lines and tubes in their body — such as a catheter or a breathing tube — are also at high risk.
How are C. auris infections treated?
Despite several strains C. auris infections being multi-drug resistant, there is a class of antifungal drugs called echinocandins that can be used and are given intravenously.
According to the National Institutes of Health, echinocandins prevent a key enzyme needed to maintain the cell wall of the fungus.
In some cases, when the infection is resistant to all three main classes of drugs, multiple high doses may be required, the CDC said.
Are C. auris infections fatal?
According to the CDC, studies are limited but anywhere between 30% and 60% of people with C. auris infections have died.
However, many of these patients also had other serious illnesses that also increased their risk of death.
“Unless there’s a break in the skin or some sort of deeper systemic infection, the risk of mortality, or some deeper complication, is relatively low unless that fungus gets in a place that it should not be,” Robert said. “For example, there’s a break in the skin, it gets in the bloodstream and there’s a Candida auris blood stream infection, and that can be quite fatal.”
He continued. “Candida auris, it sticks to everything. It can stick to heart valves and stick to catheters. I do want to emphasize that’s a rare occurrence, though.”
What can we do to prevent the spread?
There’s not much that can be done on an individual level to prevent the spread of the fungus, but the experts recommend avoiding patients with C. auris infections and that people practice proper hand hygiene when visiting at-risk populations such as hospital patients or nursing home residents.
Doron said people also need to be careful about the overuse of antibiotics. While they can be helpful in treating some infections, these medications can kill off bacteria in the gut and give more room for yeasts like C. auris to grow.
Roberts said there needs to be continued focus on equipping more labs to easily identify C. auris and focus on public health infrastructure that can identify, isolate and group patients who are infected.
“There’s many examples of this but, you know, a nursing home, a patient has Candida auris,” he said. “They spread it to their roommate, for instance. It’s really critical in that standpoint to have a mechanism to test everyone else in the nursing home to see who’s infected, put them in an isolated area, like one hallway, and put those who aren’t colonized in the other hallway.”
Roberts continued, “And if that patient needs to get admitted to the hospital, we let the hospital know this patient should be in Candida auris isolation. Don’t reuse blood pressure cuffs on that patient and go to the next patient, for instance.”
“But we don’t want people who watched ‘The Last of Us’ to think we’re all going to die,” Javaid said. “This is an infection that occurs in extremely ill individuals who are usually sick with a lot of other issues.”
Even if C. auris moves beyond health care facilities and into communities, it’s unlikely to become a problem for healthy people who do not have invasive medical devices, such as catheters, inserted into their blood vessels, Javaid said.
The main problem is preventing the fungus from spreading to patients in hospital intensive care units, Javaid said. Unfortunately C. auris can colonize not only people who come in contact with the fungus, but also patient rooms.
“By its nature it has an extreme ability to survive on surfaces,” he said. “It can colonize walls, cables, bedding, chairs. We clean everything with bleach and UV light.”
While the fungus was first identified in 2009 in Asia, scientists have determined that C. auris first appeared around the world about a decade earlier, after they re-examined older data and discovered instances where C. auris had been mistakenly identified as a different fungus, Dr. Graham Snyder, medical director of infection prevention at University of Pittsburgh Medical Center, said in an interview.
“It’s the pattern we’ve observed with these types of pathogens,” he said. “Often they start out extremely rare, then they emerge in more and more places and become widespread.”
It’s important to stop the pathogen so it doesn’t spread beyond hospitals and long-term facilities like the drug-resistant bacteria MRSA did, Snyder said.
“It’s not unusual to see MRSA in the community now,” Snyder said. “Will that happen with C. auris? I don’t know. That’s partly why the CDC is raising the alarm.”
Books can be your best pre-collapse investment.
Carnivore’s Bible (is a wellknown meat processor providing custom meat processing services locally andacross the state of Montana and more. Whether your needs are for domestic meator wild game meat processing)
The Lost Book of Remedies PDF ( contains a series of medicinal andherbal recipes to make home made remedies from medicinal plants and herbs.Chromic diseases and maladies can be overcome by taking the remediesoutlined in this book. The writer claims that his grandfather was taughtherbalism and healing whilst in active service during world war twoand that he has treated many soldiers with his home made cures. )
Easy Cellar(Info about building and managing your root cellar, plus printable plans. The book on building and using root cellars – The Complete Root Cellar Book.)
The Lost Ways (Learn the long forgotten secrets that helped our forefathers survive famines,wars,economic crisis and anything else life threw at them)
LOST WAYS 2 ( Wordof the day: Prepare! And do it the old fashion way, like our fore-fathers did it and succeed longbefore us,because what lies ahead of us will require all the help we can get. Watch this video and learn the 3 skills that ensured our ancestors survival in hard times offamine and war.)
The post Rapidly Spreading Fungus Already In 28 States, Including Illinois, Presents ‘Urgent’ Threat, CDC War appeared first on PrepperFortress.




